Fillable Do Not Resuscitate Order Template for Mississippi
Popular Mississippi Templates
Mississippi Lease Application - Specify your valid identification type and number for verification.
Mississippi Power of Attorney - This form allows you to avoid potential family disputes about medical care when you cannot voice your preferences.
The Arizona Motor Vehicle Bill of Sale form is not only a critical document for transferring ownership but also a valuable resource that can be accessed through Arizona PDFs, ensuring that both buyers and sellers have the necessary proof of transaction and vehicle details for a seamless exchange.
How to Transfer a Deed in Mississippi - Deeds often contain covenants regarding property use.
Misconceptions
Understanding the Mississippi Do Not Resuscitate (DNR) Order form is essential for individuals and families making end-of-life decisions. However, several misconceptions can cloud judgment and lead to confusion. Here are four common misconceptions:
- A DNR means you will not receive any medical care. This is false. A DNR specifically indicates that a person does not want resuscitation efforts in the event of cardiac arrest. Other forms of medical treatment and care will still be provided as necessary.
- Only terminally ill patients can have a DNR. This is not true. While many people with terminal illnesses choose a DNR, anyone can request one, regardless of their health status. It is a personal decision based on individual values and preferences.
- A DNR is a legal document that cannot be changed. This misconception is incorrect. A DNR can be revoked or modified at any time by the patient or their legal representative. Open communication with healthcare providers is crucial for ensuring that the DNR reflects current wishes.
- Having a DNR means your family will not be involved in medical decisions. This is misleading. Families often play a significant role in medical decisions, especially if the patient is unable to communicate. A DNR does not eliminate family involvement; rather, it clarifies the patient's wishes regarding resuscitation.
Addressing these misconceptions can help individuals make informed choices about their healthcare preferences and ensure that their wishes are respected.
Documents used along the form
In Mississippi, the Do Not Resuscitate (DNR) Order form is an essential document for individuals who wish to express their preferences regarding resuscitation in medical emergencies. However, there are several other forms and documents that often accompany the DNR to ensure that a person’s healthcare wishes are clearly articulated and respected. Below is a list of these important documents, each serving a unique purpose.
- Advance Directive: This legal document allows individuals to outline their preferences for medical treatment in case they become unable to communicate their wishes. It can include instructions about life-sustaining treatments and appoint a healthcare proxy.
- Healthcare Power of Attorney: This document designates a trusted person to make medical decisions on behalf of an individual if they are incapacitated. It empowers the appointed agent to act according to the individual’s wishes as expressed in their advance directive.
- Florida Lottery DOL-129 Form: This is a vital document for businesses seeking to become authorized lottery retailers in Florida, detailing application processes, fees, and requirements. For more information, visit https://floridaforms.net/blank-florida-lottery-dol-129-form/.
- Living Will: A living will is a specific type of advance directive that details the types of medical treatments an individual does or does not want in situations where they cannot express their wishes. It often addresses end-of-life care preferences.
- Physician Orders for Scope of Treatment (POST): This form translates a patient’s preferences into actionable medical orders. It is designed for individuals with serious illnesses and ensures that their treatment preferences are honored across various healthcare settings.
- Patient Advocate Designation: This document allows individuals to appoint someone to advocate for their healthcare preferences. This advocate can help ensure that medical staff understand and follow the patient’s wishes regarding treatment.
- Do Not Intubate (DNI) Order: Similar to a DNR, a DNI order specifically indicates that a patient does not wish to be intubated or placed on a ventilator. This document is crucial for those who may want to avoid invasive respiratory support.
- Emergency Medical Services (EMS) DNR Form: This form is specifically designed for use by emergency medical services. It informs responders that a DNR order is in place and should be followed during emergency situations.
- Patient Information and Medical History Form: This form provides healthcare providers with essential information about the patient’s medical history, current medications, allergies, and other relevant health details. It can assist in making informed decisions about care.
Each of these documents plays a vital role in ensuring that an individual’s healthcare preferences are respected and followed. It is crucial for individuals and their families to understand these forms and consider how they fit into their overall healthcare planning. By being proactive, individuals can ensure their wishes are known and honored during critical moments.
File Overview
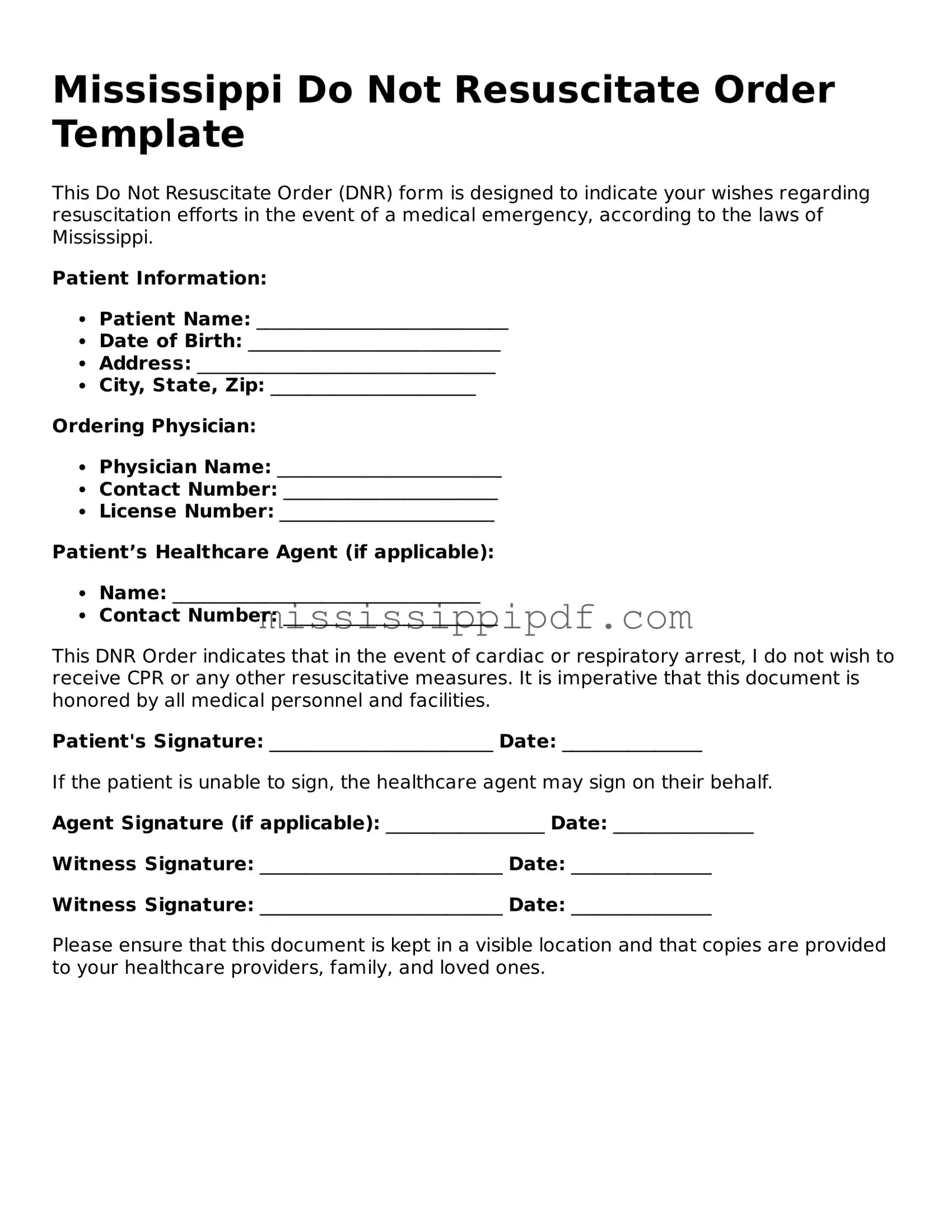
| Fact Name | Description |
|---|---|
| Purpose | The Mississippi Do Not Resuscitate (DNR) Order form is designed to inform medical personnel of a patient's wish to forgo resuscitation efforts in the event of cardiac or respiratory arrest. |
| Governing Law | This form is governed by Mississippi Code Annotated § 41-41-211, which outlines the legal framework for DNR orders in the state. |
| Eligibility | Any adult patient, or a legally authorized representative of a patient, can complete the DNR order to ensure their healthcare preferences are respected. |
| Signature Requirement | The DNR order must be signed by the patient or their representative, as well as a physician, to be considered valid. |
| Revocation | A DNR order can be revoked at any time by the patient or their representative, either verbally or in writing, ensuring that the patient's wishes can change as needed. |
Key takeaways
When filling out and using the Mississippi Do Not Resuscitate Order form, it is important to consider the following key takeaways:
- Understand the Purpose: The form is designed to communicate a patient's wishes regarding resuscitation efforts in the event of a medical emergency.
- Eligibility Requirements: Only a licensed physician can sign the form, and it must be completed in accordance with state regulations to be valid.
- Clear Communication: Ensure that the completed form is easily accessible to healthcare providers and family members to avoid confusion during critical moments.
- Review Regularly: It is advisable to review the order periodically, especially after significant health changes, to ensure it still reflects the patient's wishes.
Similar forms
The Mississippi Do Not Resuscitate (DNR) Order form shares similarities with the Advance Directive, a legal document that outlines a person's preferences regarding medical treatment in situations where they cannot communicate their wishes. Both documents allow individuals to express their desires concerning life-sustaining measures. While the DNR specifically addresses the refusal of resuscitation efforts, the Advance Directive can encompass a broader range of medical decisions, including the use of ventilators and feeding tubes. Each document serves to ensure that a person’s healthcare preferences are honored, even when they are unable to articulate them due to medical conditions.
Another document akin to the DNR is the Physician Orders for Life-Sustaining Treatment (POLST) form. The POLST is designed for patients with serious illnesses and provides specific medical orders regarding treatment preferences. Like the DNR, it is a physician-signed document that conveys the patient’s wishes to healthcare providers. However, the POLST goes beyond resuscitation preferences, detailing a comprehensive plan for other interventions such as hospitalization and antibiotics. Both documents aim to communicate a patient's wishes clearly to medical personnel, ensuring that care aligns with their values.
The Living Will is another important document that parallels the DNR Order. A Living Will outlines a person’s wishes regarding end-of-life care and is particularly relevant when a person is terminally ill or in a persistent vegetative state. Similar to the DNR, it serves as a guide for healthcare providers and family members, detailing the types of medical interventions a person does or does not want. While a DNR focuses specifically on resuscitation, a Living Will can include broader directives about life-sustaining treatments, making both documents essential for comprehensive end-of-life planning.
Healthcare Power of Attorney (POA) is also comparable to the DNR form. A Healthcare POA designates an individual to make medical decisions on behalf of another person when they are unable to do so. While the DNR provides specific instructions about resuscitation, the POA allows the appointed person to interpret and make decisions based on the patient's values and preferences. This relationship emphasizes the importance of having a trusted advocate who can ensure that the patient’s wishes are respected in various medical scenarios.
The NYC Payroll form, designed by the Department of Labor Bureau of Public Work, is a crucial tool for contractors, allowing them to meet payroll notification requirements effectively. It serves as an optional recording and submission method that captures essential employee data such as hours worked, pay rates, and deductions, thereby promoting transparency within labor practices. For those seeking more information or access to the form, resources can be found at nyforms.com/, which provides valuable templates and guidance for compliant payroll management.
The Comfort Care Order is another document that shares similarities with the DNR. This order focuses on ensuring that a patient receives palliative care rather than aggressive treatments. It emphasizes comfort and quality of life, aligning closely with the intent of a DNR, which prioritizes the avoidance of invasive resuscitation efforts. Both documents reflect a commitment to patient-centered care, allowing individuals to choose a path that aligns with their values and desires regarding their health care.
The Medical Order for Scope of Treatment (MOST) form is also relevant in this context. Similar to the DNR, the MOST form provides a clear set of medical orders that reflect a patient’s treatment preferences, especially for those with serious or chronic conditions. It is designed to be used in conjunction with the DNR, offering more detailed guidance on the level of medical intervention desired. Both documents serve to communicate critical healthcare decisions to providers, ensuring that patients receive care that aligns with their wishes.
Finally, the Do Not Intubate (DNI) order is closely related to the DNR form. A DNI specifically addresses the patient’s wishes regarding the use of intubation in the event of respiratory failure. While the DNR prohibits resuscitation efforts, the DNI focuses on the refusal of mechanical ventilation. Both documents are crucial in guiding healthcare providers about the extent of interventions a patient wishes to receive, ensuring that their end-of-life care is consistent with their personal values and preferences.